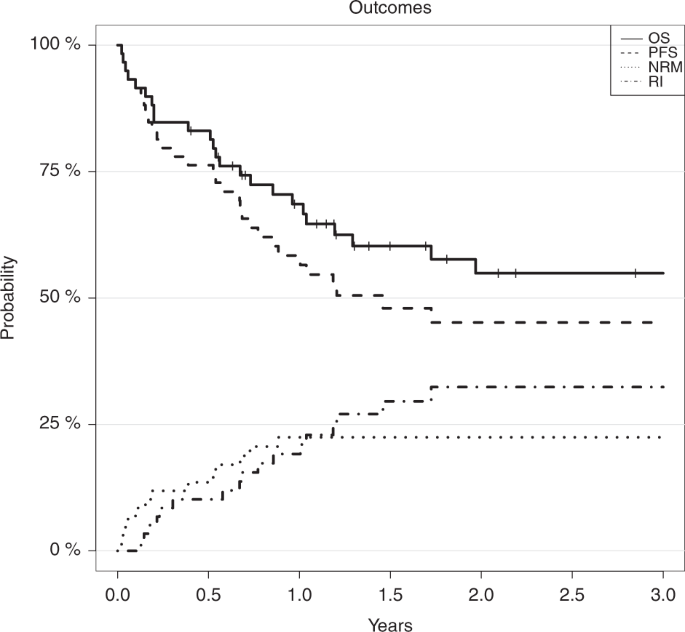
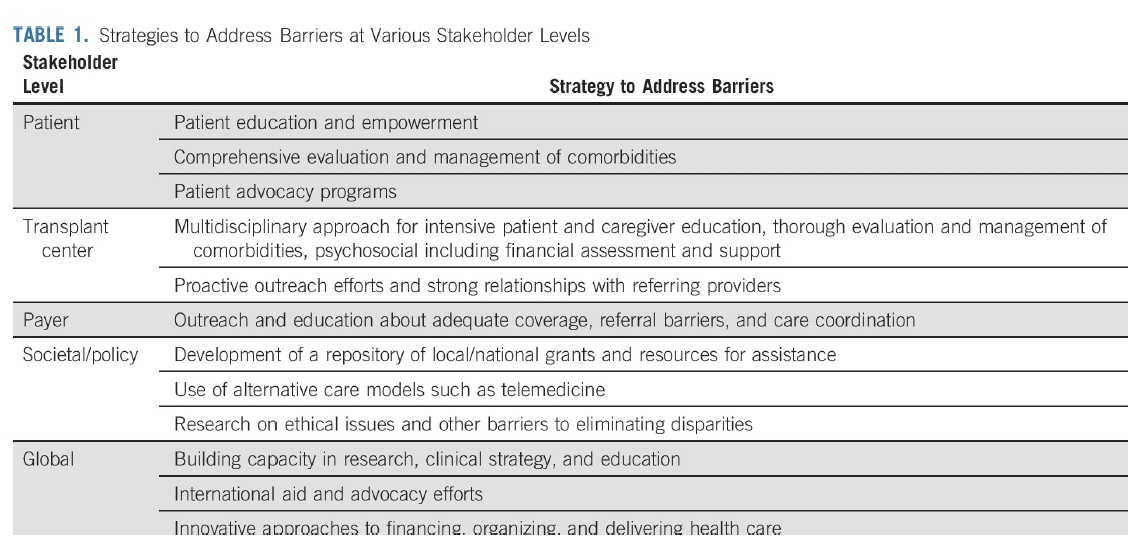
The primary goals of therapy in primary myelofibrosis mf include prolongation of survival and when possible cure which may be achieved by allogeneic stem cell transplantation.
Myelofibrosis stem cell transplant survival rate.
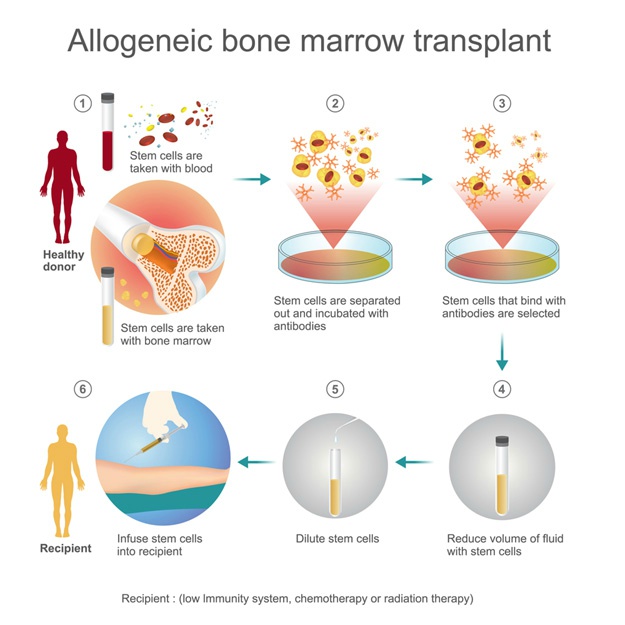
Myelofibrosis is typically treated with a stem cell transplant so i started working with uday popat m d to find a donor.
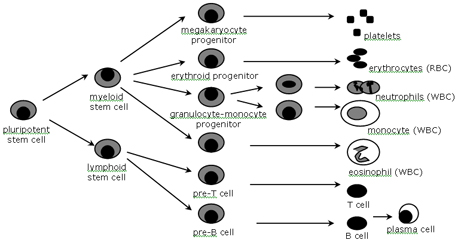
Myelofibrosis is a type of bone marrow cancer.
I wasn t in any immediate danger so we kept looking.
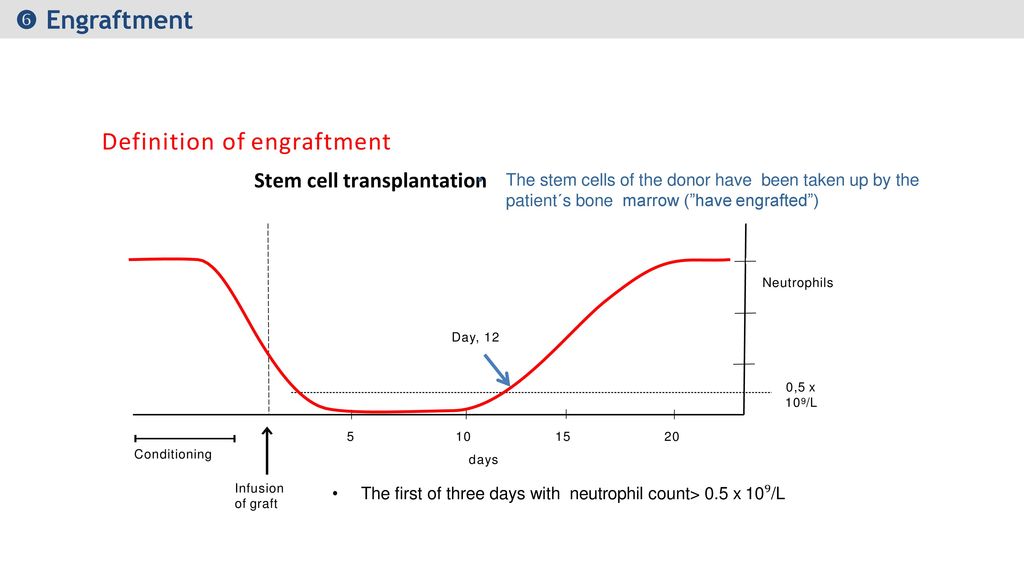
In an effort to improve stem cell transplant outcomes for mf patients mpnrf created a stem cell transplant timing tool.
Long term outcome after allogeneic hematopoietic cell transplantation for myelofibrosis published online february 2019.
It is also associated with high mortality rates which further ads to decreased life expectancy of these patients even with treatment.
Although the only cure for myelofibrosis is allogeneic stem cell transplantation relatively only few individuals are candidates for it.
Popat wanted a 100 match.
Host disease regardless.
Myelofibrosis is a rare kind of blood cancer that keeps your body from making the blood cells you need to be healthy.
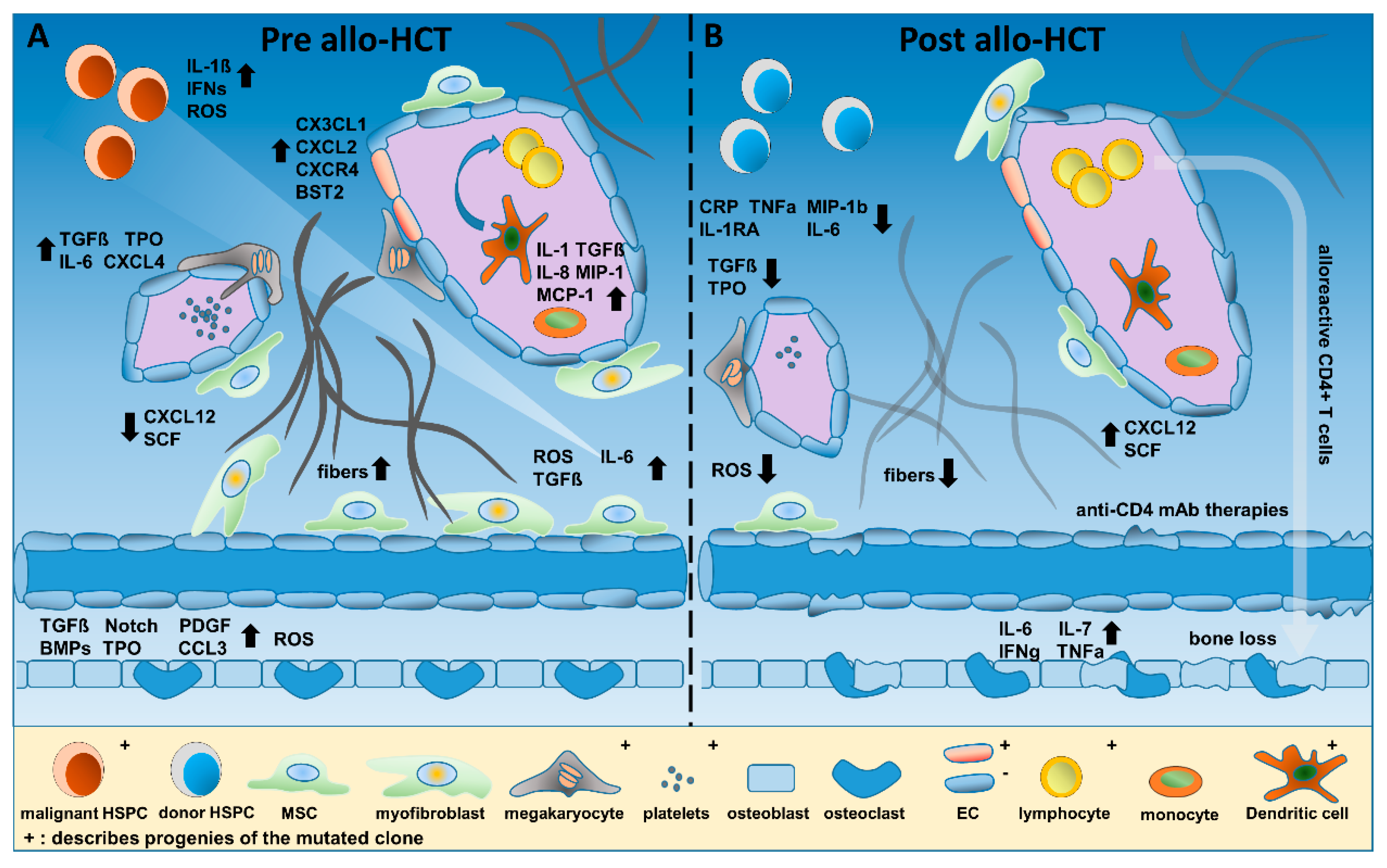
Myelofibrosis mf is a chronic hematologic malignancy characterized by clonal ineffective hematopoiesis a reactive reticulin deposition and fibrosis in bone marrow circulating cd34 progenitor cells extramedullary hematopoiesis and leukemic progression 1 mf has a heterogeneous clinical phenotype and median survival of the disease vary from 16 months to 15 years according to the dynamic.
The only treatment modality that is currently capable of prolonging survival or potential cure in mf is allogeneic stem cell transplant asct discussed in more detail below.
It provides a color signal in response to information entered by a patient that indicates a risk level and median survival times without a stem cell.
A stem cell transplant is the only treatment that can cure myelofibrosis.
Bone marrow transplants for patients with nonmalignant diseases have a much better success rate with 70 to 90 survival with a matched sibling donor and 36 to 65 with unrelated donors the life expectancy survival rate and quality of life post transplant have improved with more accurate genetic matching with donors and improved post operative care.
My sister was only a 50 match and dr.
Robin m de weede lc wolschke c et al.
35 unfortunately asct in pmf is currently associated with at least 50 rate of transplant related deaths or severe morbidity eg graft vs.
Palliation of symptoms and improved quality of life also represent important management goals.